ARE YOU OF LEGAL VAPE AGE?
Please confirm that you are of legal age to purchase vaping products to access our site.
Please confirm that you are of legal age to purchase vaping products to access our site.
Some items are no longer available. Your cart has been updated.
This discount code cannot be used in conjunction with other promotional or discounted offer.
Mr. Li, a 54-year-old man, has smoked one pack per day for 30 years. During a routine physical examination, he was shocked to learn that he had developed an 8 mm pulmonary nodule. His first questions were:
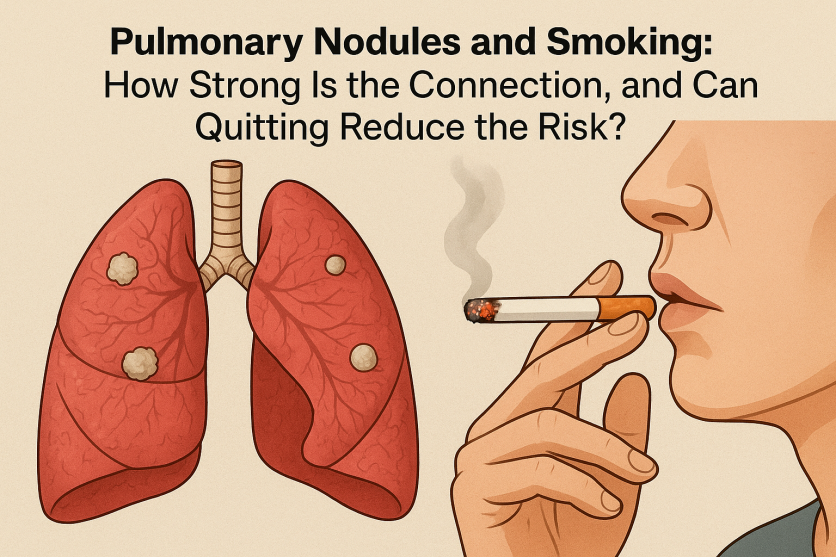
“Doctor, is this related to my smoking? If I quit now, will it still help?”
These are common concerns among long-term smokers who undergo health checks. This article reviews the scientific evidence on the relationship between smoking, pulmonary nodules, and smoking cessation.
Cigarette smoke contains more than 7,000 chemical compounds, of which at least 70 are confirmed carcinogens. These toxins continuously irritate and damage alveoli and bronchial epithelium, leading to chronic inflammation, tissue repair, and the potential formation of pulmonary nodules.
Epidemiological studies consistently demonstrate that approximately 80% of lung cancer patients have a history of long-term smoking. Importantly, many early-stage lung cancers are first detected as “small nodules” on imaging.
Smoking contributes to chronic obstructive pulmonary disease (COPD) and pulmonary fibrosis. Both conditions independently increase the likelihood of developing nodular changes in lung tissue.
👉 In summary: smokers who develop pulmonary nodules face a significantly higher probability of malignancy compared with non-smokers.
The encouraging answer is: it is never too late to quit.
👉 Even if a pulmonary nodule is already present, smoking cessation reduces the likelihood of malignant transformation and prevents the emergence of new nodules.
Smoking and pulmonary nodules are closely associated, with smokers facing a higher probability of malignant progression. However, smoking cessation significantly reduces the risk of lung cancer and the development of new nodules—even after a nodule has already been detected.
For patients like Mr. Li, the best approach combines quitting smoking, regular follow-up, and evidence-based clinical management.
Platforms like Vapepie, which provide scientifically grounded information about smoking, cessation strategies, and respiratory health, can be valuable resources for individuals seeking credible guidance and support.
If you—or a family member—were found to have a pulmonary nodule during screening and also had a smoking history, would you quit immediately, or assume “the damage is already done”? Share your thoughts; your decision could inspire others to make healthier choices.

Comment